Skin biopsy and autonomic function testing
Today I'm writing about the skin biopsy and the autonomic function testing, which I had done back in 2014 to test for small-fiber neuropathy.
What is a skin punch biopsy?
My experience with the skin biopsy
Then I had to lie on a bench on my side, so that he could get the biopsy from my leg. Already when he started, I could kind of tell that this isn't something he does very often. I'm not sure if they just don't have many people who need this exam, or if Prof. Riser usually has an assistant doing this, who deserted him on this day.😂
Prof. Riser was a bit clumsy...but he managed...
The first thing Prof. Riser had to do was to inject some lidocaine (local anesthetic) into the spot where he wanted to take the biopsy. He had these little vials of liquid lidocain, which he had to transfer into a syringe to apply it.💉
Somehow, he couldn't figure out how these vials open. So he fiddled around with one, and eventually the top popped open and half the lidocain sprayed in his face.....💦💦🙈🙈😂
Luckily it did not go in his eye and it did not seem to have done him any harm. After another try he managed to somehow open the second one properly and transferred the liquid into the syringe.
A few minutes after applying the lidocaine, he punched a whole of about 3 mm diameter and 5mm depth out of my leg. Taking the punch biopsy did not hurt at all actually.
The tissue he got out had to be transferred into a little tube filled with liquid for preservation. Somehow, this task seemed pretty difficult too and the tissue landed on the floor before it landed in the liquid....😂😩.
I don't think this would have done the probe any harm. The tissue wasn't damaged or anything. It's just funny, because he really lived up to the clichee about professors. Academically very competent but kind of confused and not very practical. It's not a bad thing, I think he knew very well what he was doing, but he probably could have used some help there.😹
I also had some autonomic function testing
Then we went on to do some additional autonomic function testing to test for small-fiber neuropathy. If you are interested in learning how small-fiber neuropathy is diagnosed, the neuropathy commons website is a good resource.
Why autonomic function testing?
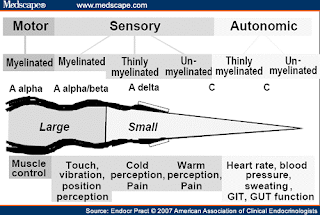
The small nerve-fibers in our bodies have several different tasks. For one, they innervate the skin where they control pain, heat regulation (by innvervating the small blood vessels), and they also control the sweat glands in the skin. Besides that, they also innervate many internal organs, where they control autonomic (unvoluntary) functions of the body, such as the heart rate, bladder control, or blood pressure.
In this figure that I found in a scientific publication, you can see what the large and small nerve fibers in our bodies do. In case of small-fiber neuropathy the sensory and autonomic fibers may be affected.
 |
|
So some people with small fiber neuropathy also suffer from tachykardia (rapid heart beat), digestive problems, bladder problems, or severely low blood pressure.
I never felt like I had any of those issues. In my case, I was just affected by pain and red swelling in my hands and feet.
Which autonomic functions did I get tested for?
He first tested the response of my heart to stress🫀🫀🫀. He measured my heart rate after lying there for a few minutes. After this he made me hyperventilate for about half a minute or so and then measured my heart rate again. Thankfully, he could not find anything wrong with my heart🫀💕.
Then he tested the response of my sweat glands to stress. I can't recall all the details, but I remember he put some electrodes on my upper body and some sort of pads to measure sweat response on my hands and feet. And once again, I got some electro shocks through my body.
Apparently when sweat glands get stressed out, for instance by electro shocks, they react by sweating. Makes sense right? ☺️And because small nerve fibers regulate sweat glands, the sweat response to electric stimuli can be reduced if you have small-fiber neuropathy.
I remember that again we had some technical complications, because somehow Professor Riser's computer died in the middle of the exam and we had to start all over.😩😩😩😩 Again, he was kind of put out of concept by the non-cooperative computer and fiddled around with many cables and adaptors and went to get support somewhere. Eventually they managed to get it up and running again, but I ended up being there for quite a while.....
All the equipment they had there kind of looked outdated. Probably shows, that skin biopsies and other small-fiber neuropathy tests were not the financial focus of the hospital, but at least they offered them. Either way, i think the Prof knew what he was doing, so I will not complain about that.
I did have abnormalities of my sweat gland reaction
Once the computer was up and running again, Prof. Riser showed me on his screen that overall my sweat response was within normal range. However, you could clearly see, that it was much less on my right foot when compared to my left foot. He repeated the test, and the results were exactly the same. Interestingly, my right foot was the one, that was a lot sorer than my left foot.🦶🏻
After that we were done and he informed me that we will have to wait several weeks for the results of the skin biopsy. But he agreed that it seemed likely that I had small-fiber neuropathy. However, he also didn't know where it came from and he agreed that an autoimmune reason is possible.
And then I finally got the prescription for some treatment to try!
I will write about my prednisone treatment in a later post, but I can tell you that much......it worked💕💥 But the time of treatment was definitely an experience in itself....
I hope you all stay well!
 Follow on Instagram
Follow on Instagram












